Seeing Clearly Now: Pioneering Steps in Space Toward a Cure for Blindness

March 25, 2025 • By Stephenie Livingston, Staff Writer
Macular degeneration is a patient thief. It doesn’t ransack your vision all at once but lifts details one by one—the fine print on a menu, the headlights on a wet road, the familiar contours of a loved one’s face. Eventually, even basic tasks become guesswork. Is that a six or a nine? A friend or a stranger? A sidewalk or an especially aggressive shadow? For millions, this is reality. The leading cause of vision loss in older adults, age-related macular degeneration (AMD), is a slow-motion heist that too often steals its victim’s independence.
And, despite decades of research, treatments remain frustratingly reactive: slow the decline, cushion the fall.
“Macular degeneration is one of those diseases where you’re constantly playing catch-up,” said Hema Ramkumar, a retinal surgeon and founder of California-based startup Oculogenex. “Patients in the intermediate stages struggle to drive at night or read fine print. By the advanced stages, they’re tethered to monthly eye injections just to keep the disease from getting worse. There’s nothing preventative. There’s no cure.”

Hema Ramkumar, Founder and CEO, Oculogenex
Media Credit: Hema Ramkumar
AMD, as the name suggests, is both age-related (most patients are over 50) and macula-related (the macula being the part of the retina responsible for sharp, central vision). It comes in two unappealing flavors: dry, which erodes vision slowly through damage from oxidative stress, and wet, which works fast and chaotically, thanks to rebellious blood vessels that bleed and scar. Wet AMD can be managed—if you count frequent, needle-to-the-eyeball injections. As for dry AMD? There’s no treatment to improve vision, no magic eye drops. It’s just a slow fade into a blurry new world.
Anatomy of the Eye
To understand macular degeneration, it helps to know a little about the eye’s anatomy. The retina is the thin, light-sensitive layer of tissue at the back of the eye. It acts like the film in a camera, capturing images and sending them to the brain via the optic nerve. At the center of the retina is the macula, a small but critical area responsible for sharp, detailed vision. Tasks like reading, driving, and recognizing faces rely on the macula functioning properly.

Age-related macular degeneration results in the loss of central vision as simulated here.
Ramkumar grew weary of delivering the same bleak prognosis, offering patients little more than a slower descent. In 2020, she found herself at a crossroads at the height of the pandemic. The pause in routine gave her time to reevaluate her path, prompting the surgeon to revisit her lifelong passion for science that began with a promise to cure blindness made at age 11 after her first eye doctor’s visit resulted in glasses. She founded Oculogenex with a bold goal: develop a gene therapy that does not just slow the disease but stops it cold—and maybe even reverses it.
“There’s a huge unmet need for therapies that can prevent or even reverse the damage before it’s too late,” Ramkumar says.
But how do you test a therapy for a disease that takes years to wreak havoc? This is an especially critical problem when you see patients every day who don’t have much time to spare. Ramkumar’s solution was unexpected, even to her: space.
This forward-thinking approach earned her a ticket to conduct a scientific investigation through the International Space Station (ISSInternational Space Station) National Laboratory. What she discovered could revolutionize our understanding of and approach to treating macular degeneration.
The Space Connection
Scientists found that the radiation and fluid shifts that occur during spaceflight create the same kind of oxidative stress in the retina that leads to macular degeneration. Oxidative stress, a damaging process caused by harmful molecules called free radicals, is the primary cause of dry AMD and is something no existing treatment effectively addresses. What’s more, astronauts, it turns out, occasionally exhibit early signs of retinal aging—a coincidence that intrigued Ramkumar.
Her lightbulb moment arrived during a MassChallenge startup accelerator program competition when someone floated the idea of leveraging the ISS National Lab to accelerate her research. The clincher? A 2019 study showing that just 35 days in low Earth orbit(Abbreviation: LEO) The orbit around the Earth that extends up to an altitude of 2,000 km (1,200 miles) from Earth’s surface. The International Space Station’s orbit is in LEO, at an altitude of approximately 250 miles. (LEO) triggered retinal changes in mice that looked eerily like the early stages of macular degeneration in humans.

SpaceX CRS-30 launches from Cape Canaveral in March of 2024.
Media Credit: SpaceX
If Earth-based scientists are hindered by long waits for AMD to develop in animal models or by the costly methods needed to induce it, space might be the fast-forward button. After pitching her idea, Oculogenex was selected for the Technology in Space PrizeA prize that provides grant funding for business startups participating in the MassChallenge startup accelerator program to conduct innovative research and technology development utilizing the ISS National Lab. The prize is funded by the Center for the Advancement of Science in Space, which manages the ISS National Lab, and Boeing., funded by Boeing and the Center for the Advancement of Science in Space®, which manages the ISS National Lab, in partnership with MassChallenge. The award recognized the potential of Ramkumar’s innovative approach to gene therapy.
The therapy employs a simple yet bold method: it uses an adeno-associated virus (AAV), a common gene delivery system, to introduce the BMI1 gene directly into retinal cells. This gene is like a molecular bodyguard, shielding the retina from oxidative stress.
Cheryl Rowe-Rendleman, a clinical development expert guiding Oculogenex through the U.S. Food and Drug Administration (FDA) approval process, emphasized the unique potential of targeting BMI1. She explained that BMI1 therapy works by rejuvenating cells damaged by the disease’s progression. It specifically alters how these cells handle energy and waste, boosting their metabolic efficiency. This enhancement in cellular metabolism is key to strengthening the retina’s cells, giving them a better chance to withstand the degenerative effects of AMD.
“Despite the myriad environmental and metabolic pressures these cells face, which could push them into an advanced stage of degeneration, BMI1 remains agnostic to these pressures,” she said. “This crucial intervention allows the patient’s cells to gain a resilience that is comprehensive and enduring.”
Ramkumar further explained, “Our goal was to design a therapy that is more robust and durable, one that doesn’t require frequent injections but instead offers long-term protection for the retina. We’re aiming for a single injection that lasts years.”

Left: Team photo after loading the flight mice for the SpaceX CRS-30 mission. Right: Hema Ramkumar and her team gather to watch the SpaceX-30 launch at Kennedy Space Center.
Media Credit: Kim Heitzman /Oculogenex
Yet, moving from theory to execution, especially in space, introduced a series of unexpected challenges. To Ramkumar’s surprise, launching an experiment to the space station isn’t as simple as slapping a FedEx label on it. After three years of meticulous planning and navigating complex regulatory requirements to test the therapy in space, Ramkumar’s team spent five intensive months at Kennedy Space Center prepping for launch on SpaceX’s 30th Commercial Resupply Services (CRS) mission for NASANational Aeronautics and Space Administration.
The goal: send 40 female mice into orbit, half treated with the gene therapy, and the other half serving as controls. But getting those 40 mice flight-ready took work—more than 300 mice were screened on the ground to ensure only the healthiest, most retinally pristine candidates made the cut.
“We tested different devices and techniques for recording retinal function, performing injections, and ensuring that the mice were stable under anesthesia,” said Zhongyang Lu, Oculogenex’s senior scientist and lab director. “It was a lot of trial and error to make sure everything was precise and ready.”
They also screened and selected 40 female mice for the ground control experiment housed at Kennedy Space Center in ISS environmental simulator chambers—miniature, ground-based replicas of the space station’s temperature and humidity conditions.
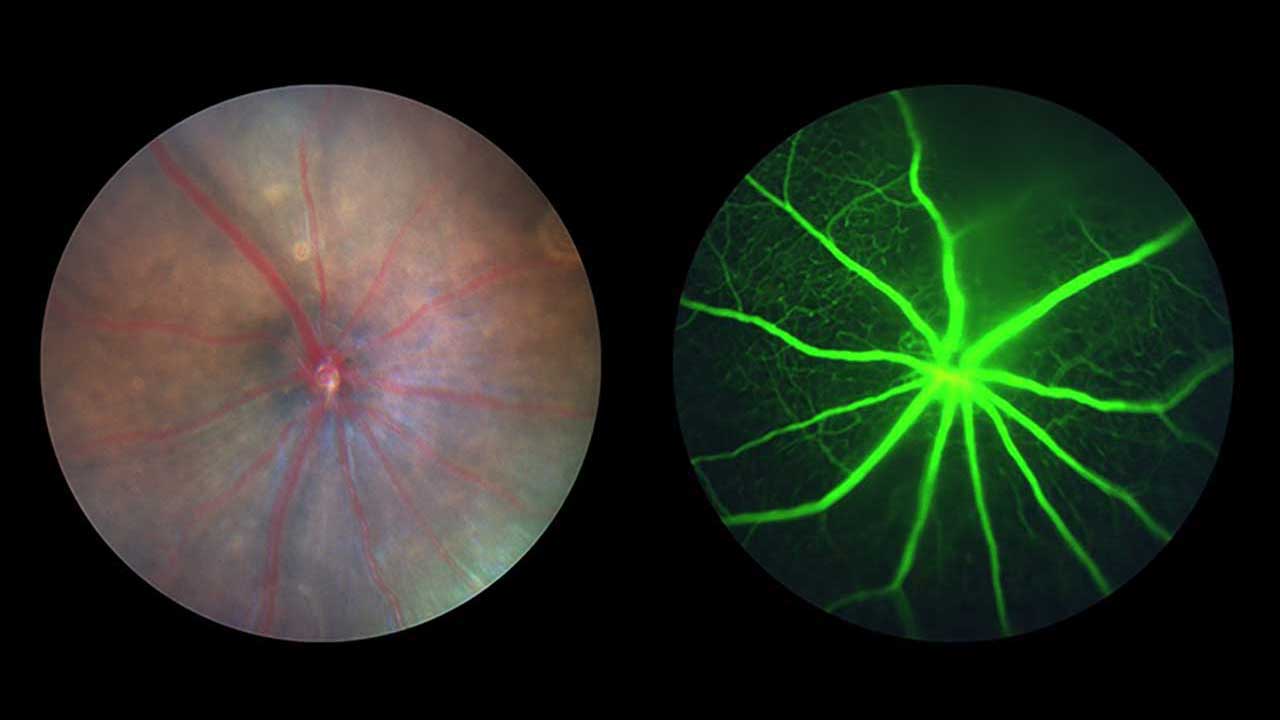
Taken with a specialized camera, images of a mouse retina before spaceflight (left) and a fluorescein angiogram, captured using a fluorescent dye, of the microvascular circulation of a mouse retina (right) are shown here.
Media Credit: Oculogenex
“The team started measurements a month before launch, using electroretinography (ERG), which is basically an EKG for the retina, and optical coherence tomography (OCT), which provides detailed images of retinal layers,” said Kristin Kopperud, science program director for the ISS National Lab, who worked closely with the team.
After a month in orbit, the mice returned safely to Earth for a battery of postflight tests—retinal imaging, electrophysiology, and tissue sampling. The data was, in a word, striking.
What did the team find? Let’s just say it was enough to make them double- and triple-check the results.
Unlocking Vision
Because AMD affects more women than men, the team sent only female mice to space to test the gene therapy. What they found was unexpected: the retinas of the mice suffered little damage from the harsh space environment.
“We think estrogen is protective,” Ramkumar said. “The hormone boosts antioxidants in the retina and mitigates stress-related damage, which might explain the surprising resilience of the female mice and offer evidence for why post-menopausal women lose eyesight to AMD.”
While this resilience complicated the team’s ability to test the damage-prevention aspect of the therapy, they did see signs of preservation compared with the control group, and it brought another revelation: improvement. “We saw a measurable improvement in retinal function after treatment,” Ramkumar said. “Not just preservation—actual improvement in how the retina works.”
That’s a surprising finding in macular degeneration research, she says. The therapy appears to enhance the retina’s bioenergetics, making cells more efficient at processing energy and oxygen. The treatment could potentially restore the cells’ health and functionality by improving these cellular functions.
“We are optimistic that this therapy will eventually reverse vision loss from AMD, a milestone we could only approach by leveraging the microgravityThe condition of perceived weightlessness created when an object is in free fall, for example when an object is in orbital motion. Microgravity alters many observable phenomena within the physical and life sciences, allowing scientists to study things in ways not possible on Earth. The International Space Station provides access to a persistent microgravity environment. environment provided by the ISS National Lab,” Ramkumar said.

Shown here is the mission patch for the team's investigation that launched on SpaceX CRS-30.
Media Credit: Oculogenex
Oculogenex is conducting critical safety studies now, with plans to develop a device to deliver the drug before identifying patients for clinical trials, which are expected to begin within the next two years, said Rowe-Rendleman.
“I’m particularly moved by the focus on a patient population with intermediate AMD, a group that has historically been poorly identified and underserved in our field,” she said. The challenge with intermediate AMD (between early and late-stage AMD) lies not only in its more subtle, sometimes hard-to-detect symptoms but also in the lack of targeted treatments, as most therapeutic advancements focus on the more severe, late stages of the disease.
It’s also not out of the realm of possibilities for Ramkumar’s research to influence how vision loss is treated beyond macular degeneration. “By educating physicians on the benefits of the BMI1 pathway,” Rowe-Rendleman says, “we could fundamentally change the approach to treating macular degeneration, offering new hope to those caught in the gap between early detection and late-stage intervention.”
For Kopperud, this study feels like an especially important one to be a part of, as it’s not just advancing science—it has a clear pathway to improving lives. “When this therapy reaches patients, it’ll be life-changing,” she says.
And what of the mice themselves? Ramkumar reports that the treated group returned from space looking notably sprightlier than their saline-injected counterparts. “Our mice were alert and active,” she said. “You could see the difference. Vision is so much more than eyesight; it’s about engagement with your surroundings.”
The team’s postflight data provided invaluable insights into how their gene therapy interacts with the stresses of space. Ramkumar said that leveraging the ISS National Lab to explore gene therapy in ways not possible on Earth paved the way for what might be a significant breakthrough in retinal medicine.
“This study gave me hope,” she said. “It reminded me why I got into this field—to change lives.”
For millions facing a slow fade to gray, it might just deliver a light switch.