The Tumor Oracle: How a Startup is Using the ISS to Outwit Cancer
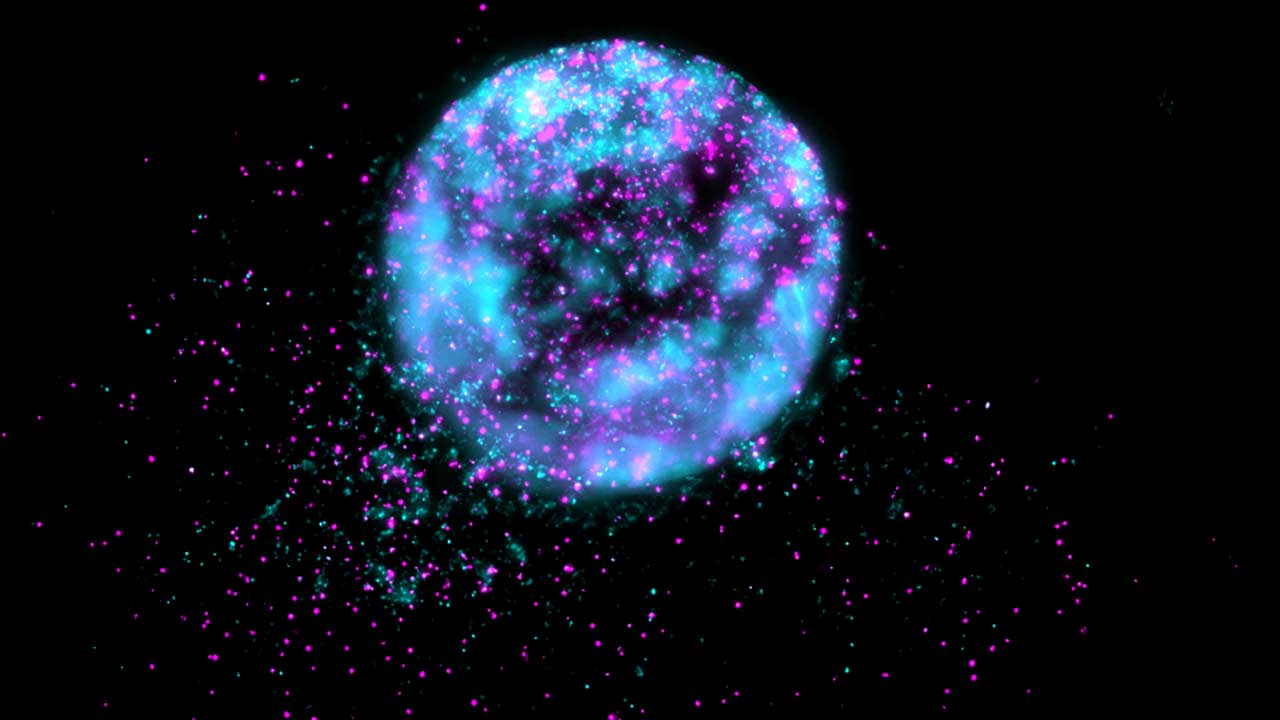
This microscopic image shows a cloned tumor sample from a SpaceX CRS-30 investigation that used Encapsulate’s tumor-on-a-chip system to grow patient-derived cancer cells and test chemotherapy drugs in microgravity.
Media Credit: Encapsulate
July 23, 2025 • By Stephenie Livingston, Staff Writer
The matte-gray box resembles a lunchbox except that you half expect steam to hiss out when the lid cracks open. It doesn’t hint at its contents: cloned tumors nestled inside clear chambers—miniature versions of real patients’ cancers, arranged like seedlings in a hydroponic tray. This tumor-on-a-chip system is a diagnostic device that sends microtumors into space to forecast how the cancer will respond to chemotherapy before the patient ever takes a dose.
Encapsulate, the Connecticut-based company that developed the system, started in a sort of orbit, circling the medical community and struggling to land an idea many dismissed as sci-fi. Armin Rad, a young biomedical engineer with a stubborn streak, co-founded the company with Leila Daneshmandi. In 2018, along with their team, they started shuttling between Connecticut and Boston, pitching the concept in scrappy accelerator sessions and to anyone who would listen: What if you could test cancer drugs on a replica of a patient’s actual tumor—outside their body—and get an answer in days?
“Everyone else was thinking that, okay, this is a crazy idea. Why are you wasting your time doing that?” says Rad.
The biotech startup originally created the platform to test chemotherapy treatments on Earth. Each chip hosts a biopsy sample—often from solid tumors like colorectal or pancreatic cancer—and grows it into several tiny, biologically identical tumors. Each microtumor gets a different pharmaceutical treatment.

A flight-ready CubeLab is tested preflight on Space Tango's emulator.
Media Credit: Space Tango
The goal? Skip the trial-and-error approach that defines much of cancer therapy, identify the most targeted treatment, and save time—time that can mean the difference between life and death. Most oncologists rely on statistical hunches: Drug A worked better than Drug B in a trial with a few hundred patients. But the patient sitting in front of them isn’t a statistic. Encapsulate wants to predict, within seven days, what will actually work for that individual.
The team could have stopped at Earth, but they encountered a problem that prevented them from accurately accessing the most drug-resistant cancers. Traditional lab models distort reality. In plastic dishes, tumor cells sprawl into single-layer sheets. Human tumors don’t behave this way. Although they could still get readings for simpler cancers, results for rare and complex ones were less reliable. They suspected gravity might be the issue and needed to escape it.
Rad found traction for his idea at MassChallenge, a global startup accelerator, where he found a potential solution. He learned that the environment on the International Space Station (ISSInternational Space Station), suspended in microgravityThe condition of perceived weightlessness created when an object is in free fall, for example when an object is in orbital motion. Microgravity alters many observable phenomena within the physical and life sciences, allowing scientists to study things in ways not possible on Earth. The International Space Station provides access to a persistent microgravity environment., encourages cells to float and self-assemble. In this weightless state, tumor cells group together and form clusters that closely mimic their behavior within the human body, providing a more accurate testing model than traditional lab cultures. The potential was too promising to ignore.

Encapsulate was presented with Technology in Space PrizeA prize that provides grant funding for business startups participating in the MassChallenge startup accelerator program to conduct innovative research and technology development utilizing the ISS National Lab. The prize is funded by the Center for the Advancement of Science in Space, which manages the ISS National Lab, and Boeing. at the 2019 MassChallenge awards ceremony (from left: Scott Copeland, Boeing; Rachel Clemens, ISS National Lab; Reza Amin, Leila Daneshmandi, and Armin Rad, Encapsulate; and Kevin Foley, Boeing).
Media Credit: Encapsulate
In 2019, Encapsulate was chosen for the Technology in Space Prize, which provides grant funding for MassChallenge participants to do research utilizing the ISS National Laboratory. With this support, the team sent the system into space—and over the course of months, everything changed. There, the tumor samples responded exactly as Rad had hoped, forming realistic 3D structures that let the team observe, in real time, how different treatments worked. It was no longer just theoretical.
“Technically, it’s not even a prediction now. It’s an observation of what would work the best on the tumor,” Rad says. “The fact is that you can save lives with this crazy idea—something people thought was impossible—and now it’s leading to something that’s never been done before.”
What They Found
A delayed launch. Months of waiting. Cold storage constraints. A pandemic. When the box finally went up, Rad watched the data come in with equal parts terror and joy. Somewhere above Earth, six tumors from six patients sat in engineered microclimates.
Encapsulate partnered with Space Tango to develop a custom, flight-ready version of their system, which installs in a power cube called a CubeLab and operates autonomously.
“The astronauts didn’t need to touch anything,” Rad said, chuckling. “Honestly, they just plugged it in like a coffee machine.”
Everything is contained in the box, he says. The tumor-on-a-chip experiments monitor temperature, oxygen, and carbon dioxide. And they show how cancer exposed to drugs behaves when you take away gravity’s effects. Then, the system watches, records, and relays the results through built-in video and software.
“What you can observe in, like, 12 months on Earth can be observed in a much shorter time— a few weeks, up to a month—up on the space station,” Rad says.
Initially, the study aimed to test three different patient-derived tumors and two drugs. COVID delays stretched timelines but provided an opportunity: more time to prepare. Encapsulate doubled the patient count and more than doubled the treatments tested before launch on SpaceX’s 30th commercial resupply services mission(Abbreviation: CRS mission) A CRS mission is a cargo resupply mission contracted by NASA to deliver supplies and research to the International Space Station on commercial spacecraft as part of the CRS contract with three commercial companies. As part of CRS missions, experiments currently return to Earth on SpaceX Dragon spacecraft that splash down in the ocean. to the ISS, contracted by NASANational Aeronautics and Space Administration.
Some results surprised them. Tumors with specific mutations responded to chemotherapy in space—but not on Earth, suggesting that microgravity unmasked hidden cellular behaviors that might otherwise go undetected. In several cases, the tumors in space took on structural features that hadn’t appeared in their Earth-grown counterparts.
“We noticed that certain mutations, such as APC, would cause certain behavior, like higher or lower sensitivity to a certain chemo drug, under microgravity that you do not see here,” Rad said
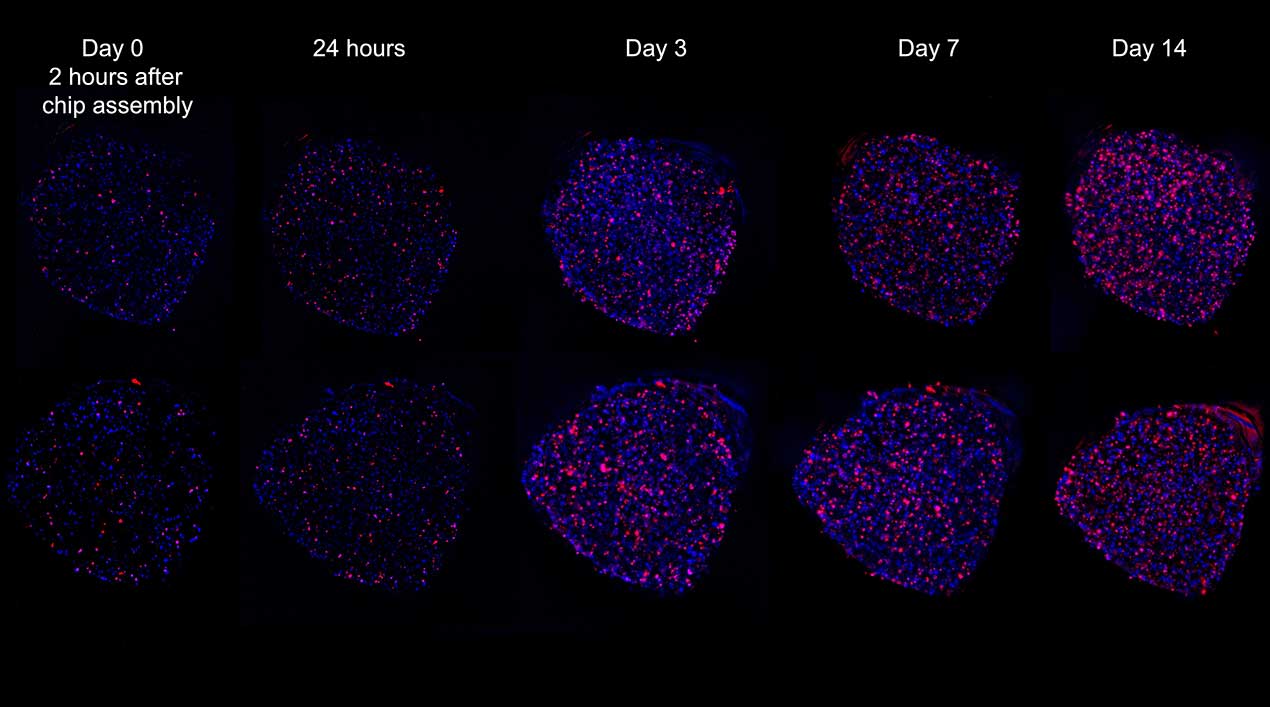
This microscopic image captures how microgravity allows tumor cells to self-assemble into clusters, mimicking their behavior in the human body.
Media Credit: Encapsulate
Strangely, some tumor-on-chip samples exhibited movement patterns that may signal early metastasis—cells from tumors known to have later spread behaved differently than those from tumors that did not. The patient’s cancer hadn’t yet spread. But in microgravity, the cloned tumor cells hinted at a future turn.
Still, the key question lingers: If tumors behave differently in orbit, how does that help a patient on Earth? The answer lies in pattern recognition. The behaviors seen in space aren’t dismissed—they’re decoded. The question isn’t whether microgravity changes outcomes, Rad explained. It’s whether those changes reveal something we couldn’t detect otherwise—that still exists in the tumor’s biology back on Earth.
The implication? The platform might not just identify a working treatment by predicting how the tumor will respond. It could warn doctors about how a tumor plans to spread.
If a tumoroid can reveal future behaviors—drug resistance and metastasis—how early does biology begin to script that story? Joel Levine, a gastrointestinal cancer specialist at UConn Health, calls it a pre-echo of metastasis.
“If I told you that you could predict that event from the day of the biopsy, you would have thought that’s counterculture,” Levine said. “But maybe we’ve been watching cancer unfold too late in the story.”
From Bedside to Space and Back
By leveraging the ISS National Lab, the team demonstrated that space-based diagnostics are achievable. Rad notes that the data they collected in orbit has already closely matched real-world results on Earth. “We monitored the same patients clinically to prove that our predictions were really happening in the clinic,” he said.
Even though the team only tested six patients, what they saw was enough to change how we think about time and tumor behavior, Rad says.
Encapsulate’s next step: a multi-site pancreatic and colorectal cancer trial. UConn Health, Moffitt Cancer Center, Memorial Sloan Kettering Cancer Center, and others plan to enroll 100 to 200 patients. Each patient’s tumor will be profiled using Encapsulate’s system. The results won’t guide treatment—yet. They’ll be compared against real-world outcomes.
Rad describes it as a low-key moonshot.
In earlier blind trials on archived samples, Encapsulate’s predictions matched clinical reality. The platform’s predictability was over 96 percent.
“It’s what the tumor does,” says Levine. “What you get out of the test of that tumor is really analogous to this being tested in you.”
Immunotherapy is up next. Unlike chemotherapy, which directly kills cancer cells, it trains the patient’s immune system to recognize and attack tumors. Although it has improved outcomes in some cancers, responses remain unpredictable. Rad’s team aims to adapt the chip to model tumor–immune interactions ex vivo, monitoring how cancer cells and immune cells interact. This will involve immune markers, co-culture systems, and advanced monitoring; however, the chip’s core architecture stays the same.
Encapsulate’s long-term plan involves using space-derived data to train AI systems on subtle cues like morphological shifts, response curves, and even behavioral signatures that precede drug resistance or metastasis. With enough examples, the system could identify the same cues in Earth-grown models (or even in imaging scans) without needing to send them to space.
Levine says this sort of precision medicine in space is challenging our understanding of the nature of cancer. “If it stays where it is and never moves, is it even cancer?” It forces you to question the basic assumptions about the ways we treat cancer, he says.
Encapsulate Scores NASA and NSF Grants
In July 2025, Encapsulate received $3.63 million from NASA’s in-space production applications(Abbreviation: InSPA) InSPA is an applied research and development program sponsored by NASA and the ISS National Lab aimed at demonstrating space-based manufacturing and production activities by using the unique space environment to develop, test, or mature products and processes that could have an economic impact. program to develop a Metastasis-on-a-Chip device onboard the ISS. The startup also secured $1.25 million from the U.S. National Science Foundation to advance its biochip platform, which screens drugs on patient-derived microtumors to personalize cancer treatment, with clinical studies planned for pancreatic and colorectal cancers.
For Encapsulate, low Earth orbit(Abbreviation: LEO) The orbit around the Earth that extends up to an altitude of 2,000 km (1,200 miles) from Earth’s surface. The International Space Station’s orbit is in LEO, at an altitude of approximately 250 miles. isn’t just a research venue—it’s clinical infrastructure. The company envisions a tiered system: standard cases stay on Earth, while the toughest, drug-resistant tumors get a ride to space for analysis in microgravity. Only about 10-15 percent of cancers would require this specialized testing; most patients could be treated using Earth-based models. Space, meanwhile, provides advanced profiling where existing tools fall short. Although capacity is limited, partnerships with firms like Space Tango aim to make the system more automated, compact, and affordable. Within 5 to 10 years, these advancements could enable scalable testing for patients who need it most.
It sounds extravagant—until you tally the cost of advanced cancer care. Encapsulate pegs its method at a few thousand dollars per patient. By contrast, late-stage cancer treatment often runs more than $500,000.
Matthew Strickland, a GI oncologist at Mass General, envisions a day when a single biopsy triggers two returns: pathology and a treatment profile. The system, ideally, tells him what works before he writes the first prescription.
“I dream about a future where the tumor has been sent to a laboratory where a model fully representative of that patient’s tumor has been established and is growing on a chip. Further, the drugs that work and don’t work have already been tested,” Strickland said.
Strickland has flown his experiments onboard a SpaceX rocket to the space station. His early data suggest that microgravity may blunt apoptosis, the cellular self-destruct mechanism that many cancer treatments rely on. His lab recently completed RNA sequencing on tumors grown in space.
“I think that the symbolism is that there are no limits to how far we’re going to go and explore to discover new therapies for patients,” Strickland said. “Even to space.”

The team prepares flight samples for SpaceX CRS-30 at Kennedy Space Center (from left: Mark Reeves, Zach Jacobs, Kendall Nelson, and Taylor Stallings-Pinnick, Space Tango; John Catechis and Erica Bumgardner, ISS National Lab; and Armin Rad, Encapsulate).
Media Credit: Encapsulate
Whether those microgravity behaviors hold the key to understanding cancer in the human body remains to be seen. Rad doesn’t speculate. He points out that six patients are a small sample, and there’s still a long road ahead. But the early signal is this: A tumor’s intent might not be random. It might be clocked early—early enough to pick the right drug to fight it, possibly before symptoms appear and before it spreads.
He wants to know what happens when we shrink more cancers into a chip, shoot them into space, and see what they have to say for themselves.
Perhaps, if Rad gets his way, cancer itself will become less mysterious, Levine says. Or maybe it becomes something else entirely: predictable, treatable—telling us from the start what it will do.
“Everything starts in a place you cannot see. Remember that. Then you light it up and you say, that was always there. I just didn’t see it.”